A Global NCD Agenda for
Resilience and recovery from
COVID-19
3 PILLARS : 12 RECOMMENDATIONS
Executive Summary
A GLOBAL AGENDA TO RESPOND TO TODAY’S CRISIS, PREPARE FOR TOMORROW’S THREATS
The 12 recommendations outlined in this Agenda are grouped into three pillars:
Pillar 1 - Governance: Redefine priorities and power and measure what matters
- Include NCDs in COVID-19 response, recovery, and preparedness plans
- Involve the community in decision-making
- Rethink the investment case for NCDs, putting a value on security and equity
- Redefine how health security and pandemic preparedness is measured
- Redress conflicts of interest and power imbalances
Pillar 2 - Prevention: Prioritise health as a path to preparedness
- Pivot to prevention
- Combat inequalities through better social protection
Pillar 3 - Health systems: Fairer and fit for the future
- Integrate NCD services into the pandemic response and beyond
- Strengthen health services and primary care at the community level
- Anchor innovations in data and deployment of digital technologies
- Resolve bottlenecks in supply chains
- Facilitate and support local production of essential NCD medicines
This Agenda is guided by the principles of equity, quality of care, and putting people first. The recommendations are informed by expertise from global health experts, including people living with NCDs and civil society organisations.
Acknowledgements: The NCD Alliance wishes to thank our members and the Our Views, Our Voices Global Advisory Committee for their invaluable inputs. We are grateful to members of the expert advisory group for their guidance and support: Sir George Alleyne, Director Emeritus Pan-American Health Organisation, Barbados; Martin Bernhardt, Sanofi, Switzerland; Professor Agnes Binagwaho, Vice Chancellor, University of Global Health Equity, Rwanda; Richard Gregory, WHO, UHC2030, UK/Switzerland; Paula Johns, ACT+, Brazil; Fale Andrew Lesā, NCD Child, Samoa/New Zealand; Dr Andrew Schroeder, Direct Relief, USA; Dr Sudhvir Singh, the Independent Panel for Pandemic Preparedness and Response, New Zealand/Norway. In addition, our thanks to Ademola Osigbesan from UNITAID for his review.
Policy Context
The syndemic of COVID-19 and noncommunicable diseases
COVID-19 has shaken the foundations of health systems and economies worldwide and up-ended the understanding of what it takes to be prepared for a pandemic. The response in the countries thought to be best prepared for an epidemic was undermined by an underestimated threat, previously overlooked in health security rankings: non-communicable diseases (NCDs). People living with NCDs have been at the epicentre of this crisis in low- and high-income countries alike. High prevalence of NCDs has caused increased mortality and morbidity in people with COVID-19, has put large sections of the population at risk and has destabilised health systems as a result. It has become indisputable that governments and global institutions are facing a syndemic, where the acute pandemic of COVID-19 is compounding the impacts of the chronic pandemic of NCDs.[1]
With this crisis, we must utilise this window of opportunity to not work in siloes but collaborate on building up a stronger financed public health system where we must prepare to fight the health disparities and make a reasonably just society for all. Access to care for people living with NCDs is quintessential and must be integrated into the health systems to combat the double burden of diseases over the years. The adversities due to the pandemic really have jolted health systems and really involve the collaboration of civil societies and publichealth to work together to build back better.”
Two categories of disease are interacting within specific populations—infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and an array of non-communicable diseases (NCDs). These conditions are clustering within social groups according to patterns of inequality deeply embedded in our societies. The aggregation of these diseases on a background of social and economic disparity exacerbates the adverse effects of each separate disease. COVID-19 is not a pandemic. It is a syndemic.”
In addition, people living with NCDs are experiencing the collateral damage of the pandemic, due to
severe disruptions to essential health services, as important elements of health systems including workforce have been redeployed to respond to COVID-19.[6] The toll is still rising from postponed treatments for stroke, cardiovascular or kidney disease, delayed diagnoses for cancer, supply chain failures
for lifesaving medicines such as insulin, suspension of rehabilitation, palliative care and mental health services (which were disrupted in 93% of countries reporting to WHO) and oral health services. But it
is certain that the overall impact on health in every country will be far larger than that of the virus itself.
The Institute for Health Metrics and Evaluation (IHME) has estimated that, as of 13 May 2021, there have
been 7.1 million deaths attributable to the pandemic.[7] This is more than double the reported number of 3.3 million COVID-19 deaths. The difference is explained by several factors, including premature deaths
due to delayed or deferred healthcare, increases in mental health conditions, and increased alcohol and drug use, as well as potential under-reporting.
Inequalities within and between countries are reflected in the burden of NCDs and are further highlighted by the differing toll of COVID-19 among different population groups. Both NCDs and COVID-19 disproportionately affect people who are marginalised and discriminated against, due to deprivation, employment status, age, race or ethnicity. [8]

Source: IHME Estimation of excess mortality due to COVID-19 | Institute for Health Metrics and Evaluation (healthdata.org) i
COVID-19 has brutally exposed entrenched inequity and injustice in all societies. People in deprived communities are also on the frontlines of the economic impact and faced with the toughest choices due to restrictions on movement, work and social interaction. These inequalities are being further exacerbated as governments and the international community fail to deliver an equitable COVID-19 response, not least regarding access to vaccines. International commitments to prioritise the most vulnerable and leave no one behind are not yet reflected in the response.
It’s not just COVID-19 that is killing people, it’s underprivilege, it’s lack of access, it’s years of living with health conditions that haven’t been properly managed because of the colour of your skin, or your ethnicity, or your social group.”
i IHME: “Excess mortality is influenced by six drivers of all-cause mortality that relate to the pandemic and the social distancing mandates that came with the pandemic. These six drivers are: a) the excess COVID-19 death rate, that is, all deaths directly related to COVID-19 infection; b) the increase in mortality due to needed healthcare being delayed or deferred during the pandemic; c) the increase in mortality due to increases in mental health disorders including depression, increased alcohol use, and increased opioid use; d) the reduction in mortality due to decreases in injuries because of general reductions in mobility associated with social distancing mandates; e) the reductions in mortality due to reduced transmission of other viruses, most notably influenza, respiratory syncytial virus, and measles; and f) the reductions in mortality due to some chronic conditions, such as cardiovascular disease and chronic respiratory disease, that occur when frail individuals who would have died from these conditions died earlier from COVID-19 instead. To correctly estimate the excess COVID-19 mortality, we need to take into account all six of these drivers of change in mortality that have happened since the onset of the pandemic.”

© Shutterstock
Recommendations
Transformative priorities, policies and public spending to build resilience
Governments and international institutions have an opportunity to act on common drivers of the syndemic of NCDs and COVID-19. Over one quarter of the world’s population live with one or more NCDs which put them at higher risk from COVID-19..[9]
This can no longer be neglected in response and preparedness for future health threats. A key to recovering stronger is to keep populations in better health, by ensuring that NCDs are more effectively prevented, diagnosed, managed, and treated. This requires tackling the structural factors (socio-economic, environmental, commercial, political) underlying both COVID-19 and NCDs in every country and across all age groups. This includes poverty and inequalities, barriers to accessing quality healthcare, and the preventable harm caused by tobacco, alcohol, ultra-processed food and drinks, and pollution.
This agenda presents 12 policy recommendations under three pillars for transformative action: Governance, Prevention and Health Systems.
Pillar 1
Governance: Redefine priorities and power and measure what matters
The COVID-19 pandemic has illustrated the importance of whole-of-government responses. This entails Heads of Government and all Ministries and departments deploying coherent measures to contain the virus and mitigate its impacts, as far as possible, on all sectors, including health, social care, the economy, employment, education, and trade. The first set of recommendations presented here therefore focuses on how decision making and governance can be improved.
To serve communities in a more equitable manner and promote healthy societies, resilience must be developed with these communities and according to their needs. There can be no health systems resilience without community engagement across domains.”
If there’s one lesson we have learned from COVID, it’s the role of communities and civil society at the national and global level.”
RECOMMENDATION #1
Include NCDs in COVID-19 response, recovery, and preparedness plans
National plans for response, recovery and preparedness should be designed around their community’s most pressing needs.
In the UN General Assembly 2020 resolution on COVID-19, governments committed to “further strengthen efforts to address NCDs as part of Universal Health Coverage (UHC), recognising that people living with NCDs and those exposed to major risk factors are at a higher risk of developing severe COVID-19 symptoms and are among the most impacted by the pandemic”.[11] To date however, only 16 countries have reported that NCD management in essential health services is included in national COVID-19 response and recovery plans.
Responding to the community’s most urgent health needs requires resuming and seizing the opportunity to improve on NCD and mental health services – including prevention, screening, diagnosis, treatment, rehabilitation and palliative care – as a matter of urgency, in order to minimise further preventable suffering. Severe disruptions to NCD care, including screening and diagnosis, are significantly increasing the death toll during the pandemic. The disruptions are creating huge backlogs in numbers of people waiting for care, across all NCDs and mental health conditions.
Special consideration is required for marginalised groups and the most deprived populations, where risk factors for communicable diseases and NCDs are compounded. This includes 68 million people worldwide currently living in humanitarian settings, displaced by conflicts and natural disasters, such as communities acutely impacted by climate change. This is accompanied by rising demand for NCD care and mental health services and is projected to keep increasing. The needs of people living with NCDs in these settings requires international support for an improved response in primary health care within national health systems, including access to community health workers, diagnosis, treatment and medicines for chronic NCDs, as well as safe living conditions, nutritious food and good sanitation.
Inspiring Examples
Bahrain is recognised for linking action on NCDs into the national recovery plans, thanks to the engagement of the Director for NCDs at the Ministry of Health in their national COVID-19 response committee.
In Ghana, the President used several televised national addresses on COVID-19 to raise awareness of NCDs and major risk factors

© Shutterstock
RECOMMENDATION #2
Involve the community in decision-making
In order to understand people’s needs, community engagement must be enshrined in national response and recovery plans and in the development and outcomes of the pandemic treaty, requiring decision-makers to include those at highest risk.[12]
This includes people living with chronic conditions, including NCDs, disabilities, HIV, TB and ‘long COVID’. Decision makers must also consciously reach out to groups too often left behind: Older people, racial and ethnic minorities, Indigenous communities, people living in urban slums, rural or remote communities, small island developing states, and LGBTQ+ and other marginalised groups. Women are being particularly hard hit by the economic impacts of the pandemic and millions of children and youth are living with NCDs (for example, over 4.5 million children and youth are living with diabetes[13]). They must also be given special consideration in community engagement.
The Independent Panel on Pandemic Preparedness and Response found that the most successful national responses to COVID-19 have been those which engaged with local communities to build resilient health systems, and to inform service delivery, decision-making and governance to meet communities’ needs.[14] Governments committed at the UN High-Level Meeting on UHC in 2019 to establish social participation mechanisms for health decision-making.[15] However, engagement of communities and civil society is still insufficient. Recent trends in many countries to shrink civil society space provide fertile ground for mistrust, which threatens public health.
Engaging diverse groups across the community will increase buy-in to policy responses and decrease health inequalities within countries, and should be a cornerstone of recovery. The pandemic has demonstrated the vital importance of public trust. Lack of trust undermines policy responses and increases inequalities, by reducing adherence to public health guidance, hindering uptake of vaccinations, and dissuading people from seeking timely health care. Participation from across the community in decision-making is an essential foundation to embed trust, combat misinformation, and close the perceived distance between public authorities, health systems and the public.
During the COVID-19 pandemic, many civil society organisations (CSOs) and health professional associations have stepped in to offer support to people living with NCDs where public services were not available, including home delivery of medicines, transporting people to hospital appointments, and offering advice and support. This should be supported by sustainable resources to work alongside governments in formulating and implementing response and recovery plans based on their experience.
Inspiring Examples
NCD civil society and patient representatives in the Philippines, including Cancer Warriors Philippines, are represented on the national advisory council on medicines, and have been involved in emergency meetings on the COVID-19 response.
In India, Blue Circle Foundation (member of Healthy India Alliance) mobilised volunteers to ensure that people living with diabetes were supported; for example, via dedicated helplines to seek advice, or to have essential medication delivered directly to their homes.
When health systems succeed we thrive; when they fail we pay with our lives. All health systems should prioritise the valuable inclusion of persons with lived experience with communicable and noncommunicable diseases in all health policy development and implementation, including the COVID-19 response and Universal Health Coverage.”
GLOBAL CHARTER
The Global Charter on Meaningful Involvement of People Living with NCDs provides fundamental principles and common strategies for placing people living with NCDs and communities at the centre of the NCD response. Policymakers are encouraged to endorse the Global Charter, recognising that the voices of people living with NCDs, with communities and a strong civil society are an imperative to achieving health and development goals – at global, regional, national and local levels.
RECOMMENDATION #3
Rethink the investment case for NCDs, putting a value on security and equity
International financing for the COVID-19 response was mobilised too late and remains too little to provide the “dangerously underfunded” global public goods identified by the Independent Panel for Pandemic Preparedness and Response and the G20 High-Level Independent Panel on Financing the Global Commons for Pandemic Preparedness and Response.[16]The same could be said for NCDs, which remain the biggest causes of premature death and disability worldwide, but currently attract less than 2% of global health financing.[17]
The NCD Alliance supports the recommendations of the panels on global mobilisation of necessary financing to protect against pandemics, but emphasises that investments for the pandemic response must not create another disease-specific silo. A siloed approach risks further exacerbating inequality and inefficiency. Longstanding silos in global health, with funding and health workers restricted to certain disease responses or specific population groups, do not sufficiently recognise the cross-cutting benefits of investments in primary healthcare and NCD prevention. The pandemic brings home the overdue lesson that the same people affected by or at risk of infectious diseases also have broader health needs, including NCDs and mental health.
Heads of Government, Ministries of Finance and international institutions should examine the investment case for making NCDs central to planning, considering the value of healthy, resilient and productive populations as an indispensable asset and of averted future health costs of both NCDs and infectious diseases. This investment case should guide domestic resource allocation, fiscal policies, development assistance, and specific international solidarity mechanisms such as the Health Systems Connector within the ACTAccelerator (Access to COVID-19 Tools), coordinated by Global Fund, World Bank and WHO.[18]
In light of the experience of the syndemic of NCDs and COVID-19, governments and international donors should accord a significantly higher value to the investment case for public health and NCD policies. The WHO set of recommended NCD interventions should be further strengthened and expanded, reflecting the value of improved security and resilience, and reduced inequalities in the cost-benefit analysis. Expansion to include policy recommendations to reduce air pollution and improve mental health is overdue and should be accelerated in light of the severe impacts of the pandemic on community mental health and in regions with poor air quality. The investment case for NCD prevention policies (including within other global health priorities such as maternal and child health, and people living with and at risk of HIV, TB or malaria) should also take into account wider health co-benefits and prevention of complications and co-morbidities, which dramatically increase the cost of healthcare and vulnerability to infectious diseases.[19]
Inspiring examples:
Bhutan is developing a national multisectoral action plan on NCDs, recognising the link between COVID-19 deaths and NCDs, and including consideration of fiscal measures on key risk factors for cardiovascular disease and diabetes.
Philippines has continued to increase the share of taxes raised from tobacco products during the COVID-19 pandemic, with a share being earmarked to bolster capacity for UHC to reach the poorest communities.
India’s budget for the fiscal year that begins 1 April 2021 more than doubles national healthcare and wellbeing spending to 2.2 trillion rupees (US $30.1 billion). It is allocated to develop capacity for primary, secondary and tertiary care, strengthen the National Center for Disease Control, and improve sanitation and air quality.
We welcome the commitment to increase domestic financing and development assistance in achieving Universal Health Coverage. UHC is really far off because it doesn’t reach all people. There is a gap between commitment and action, until this gap between commitment made and action is closed, the world will continue to bear the burden of disabilities and deaths from NCDs.”
Health systems should be reimagined in light of the pandemic… and better serve the purpose of preparing for and responding to anticipated (and unanticipated) future hazards and risks, and to produce healthier and more resilient societies. …Reconceptualising health systems means shifting future investments into these functions to strengthen health systems and prevent further fragmentation of competing parallel investments in health security and health promotion.”[20]
RECOMMENDATION #4
Redefine how health security and pandemic preparedness is measured
COVID-19 has demonstrated once again, following observations during the SARS and MERS epidemics, that people living with NCDs are at higher risk and people living with multiple NCDs are the most vulnerable during health crises.
For example, systematic reviews and meta-analysis have demonstrated that people living with obesity linked to cardiovascular and metabolic conditions including hypertension and diabetes, have up to seven times higher risk of severe disease, hospitalisation and death from viral infections including COVID-19 and influenza.[21][22] Similarly, tobacco users are at higher risk of a number of NCDs, including cancer, cardiovascular disease and lung disease, and are found to be at higher risk of severe outcomes from COVID-19. People with gum disease also have more severe outcomes from COVID-19 and have up to nine times higher risk for death, four times higher risk for intensive care unit admission and five times higher risk for assisted ventilation.[23]
To date, the International Health Regulations, WHO’s Health Emergencies pillar, and the Global Health Security Index have not considered the extent to which NCD prevalence exposes populations and economies to unnecessary risk. When aiming to strengthen health systems, governments have tended to focus either on a health security approach or a UHC one, but these should not be considered as mutually exclusive alternatives.[24] Policymakers missed the opportunity to manage and mitigate the vulnerability to epidemics by acting on common risk factors, including NCDs, by providing UHC. While the World Bank and WHO have recognised population health as an economic asset in the concept of human capital, this has not gained widespread traction to shift the political mindset.
As around half of NCDs are preventable via action on common risk factors (tobacco and alcohol use, air pollution, physical inactivity and consumption of unhealthy and ultra-processed food and drinks), governments, international institutions and preparedness rankings must recognise communities that are highly exposed to these risks, which increase vulnerability to future epidemics.
It is therefore imperative to include NCD indicators in surveillance and periodic universal peer reviews of national pandemic preparedness and response capacities. Scoping is underway on how to integrate NCDs into updates of the Global Health Security Index and should also be incorporated into international assessments of preparedness being discussed in the context of a potential pandemic treaty. For example, the data reported to WHO under the NCD global monitoring framework can be used for this purpose. Where not already the case, NCD prevalence and risk factor data should be included in health management information systems to inform decisions on health systems strengthening and NCD prevention policies.
Inspiring examples:
In recognition of the connection between obesity prevalence and population risk of COVID-19, new policy action on obesity has been announced in the United Kingdom. In the UK, it has been found that over a third of COVID-19 hospitalisations can be attributed to lack of physical activity and excess bodyweight.[25]
RECOMMENDATION #5
Redress conflicts of interest and power imbalances
The pandemic has accelerated recognition that imbalances in power and concentration of wealth continue to unduly influence decision-making. Putting short-term economic interests ahead of public health has cost lives and livelihoods.
The inequitable access to COVID-19 vaccines, both between countries and between communities, shows that stronger international governance mechanisms are needed for fairer pandemic responses. In addition, environmental destruction and pollution continue unabated, which put the world at risk of further avoidable health security threats, including climate change, biodiversity collapse, transmission of zoonotic diseases and antimicrobial resistance. Each of these could trigger humanitarian and economic crises at an unprecedented scale. The development of a pandemic treaty offers an opportunity for improved governance to address health threats and mobilise both national and international resources for global public goods. The world must not return to businessas- usual, but reset with health as the bottom line.
There are broader structural questions to address in relation to governance and planetary health. Case studies from all continents have demonstrated that health-harming industries – including ultra-processed food and drink, alcohol, tobacco, and polluters – have exploited the pandemic to gain unhealthy influence over consumers and decision-makers.[26] The pandemic demonstrates the urgency of redressing these power imbalances and an opportunity for dialogue with the public about better protecting their interests and responding to their health concerns.
The political influence of industries and companies whose practices and products are harmful to health must be closely monitored and strictly limited. Governments must be empowered by better governance to reverse the regulatory ‘race to the bottom’ and put public health first, to close cross border tax loopholes, levy taxes on health-harming commodities and phase out health-harmful subsidies, including those which incentivise production and promotion of tobacco, alcohol, ultra-processed foods and drinks, and fossil fuels. The resulting revenues and savings should be used to build back fairer – for health protection and health promoting commodities and public services.
Inspiring examples:
The pandemic has catalysed solutions in the field of planetary health:
Proposed in the context of the pandemic, the European Union will adopt a legislative package to deliver on climate targets and become the first carbon neutral continent, noting “This decade is a make-or-break moment for delivering on our commitments under the Paris Agreement, in the interest of the health, wellbeing and prosperity of all.[27] The European Union institutions operate a Transparency Register to monitor and publish lobbying activities.[28]
In the Pacific Islands efforts are being intensified to bring back traditional eating habits and reduce the consumption of unhealthy imported products. The government in Fiji for example began distributing seeds to residents during lockdown to ensure a secure supply of healthy food, in a country where only 16% of the population is aged more than 55 years due to premature deaths primarily caused by NCDs.
In Namibia, Zambia, South Africa and Sierra Leone, people living in urban slums are receiving support for local gardening and permaculture projects to promote nutritious food security and bolder livelihoods.[29]
In
Bogota, Paris and London, mayors are investing to increase the network of safe bicycle lanes to keep people active and reduce crowding on public transport. As a healthy side effect, this addresses two of the five major NCD risk factors – air pollution and lack of exercise.

© Shutterstock
Pillar 2
Prevention: Prioritise population health as a path to preparedness
A healthy population is the foundation for security, resilience, preparedness for health threats and economic development. It is therefore vital to invest in health promotion, NCD prevention, screening and diagnosis as part of the pandemic response, recovery and future preparedness. Increased attention to at-risk groups and closing the diagnosis gap is a major blind-spot to be addressed, as early diagnosis allows further complications and comorbidities to be prevented.[30] For example, half of adults living with diabetes are undiagnosed and even in high-income countries only one in five people living with hypertension is under medical control. People living with hypertension, diabetes and/or chronic kidney disease experienced barriers to accessing care and worsening of symptoms during the pandemic, often coupled with significant loss of income and employment, and widening health and socio-economic disparities.[31] [32]
Those living with NCDs are particularly vulnerable. The full extent of this may be unknown, due to the many cases of NCDs that go undiagnosed. The prevention and control of NCDs therefore has a crucial role in the COVID-19 response. If the COVID-19 response is not adapted to encompass prevention and management of NCD risks, we will fail many people at a time when their vulnerability is heightened.[33]
RECOMMENDATION #6
Pivot to prevention
The pandemic presents an imperative to reset and reorient policies to build back fairer, and smarter. Both COVID-19 and NCDs represent devastating losses in human terms, and of countries’ most valuable resource – the ingenuity, creativity and productivity of their people.
Leaders must shift their priorities to achieve healthier populations, accompanied by resources and political capital to invest in prevention of diseases. Recovery policies must achieve a step change to societies and environments that promote health and wellbeing. Much of what is needed is outside the remit of ministries of health, and involves economy, trade, environment, energy, transport, urban development, agriculture, and food systems, so leadership has to come from the top of governments. This includes implementing legislation and regulation which has proven cost-effective in preventing a range of NCDs – the set of evidencebased WHO recommended interventions.[34]
Maintaining and improving population health will guard against future health threats and reduce the costs of future health crises. Several of the major risk factors for NCDs increase the risk of severe illness and mortality from COVID-19, including tobacco use, unhealthy diet and insufficient exercise (overweight and obesity), and exposure to air pollution. NCDs have exposed countries to unnecessary risk during disease outbreaks, but many NCDs can be effectively prevented. Tobacco, air pollution and diet-related NCDs are now each estimated to cause around eight million premature deaths worldwide every year, with a further three million deaths associated with alcohol use. Most of this human and economic cost, including costly complications and comorbidities can be averted via tried-and-tested policies.[35]
In several countries, the pandemic has already catalysed important policy changes; for example, introduction of front-of-pack warning labels for unhealthy foods, supporting active transport in cities, levying higher taxes on tobacco and sugarsweetened drinks, bans on industrially-produced trans fats, restrictions on retail availability of alcohol, bans on advertising and selling junk food in schools, and measures to reduce air pollution.
Inspiring examples:
Recognising a disproportionate number of COVID-19 cases amongst overweight children and adults, the Mexican states of Oaxaca and Tabasco banned the sale of junk food and sugary drinks to unaccompanied under 18-year-olds in 2020, with more states planning to follow suit. A Mexican nationwide front-of-packaging warning labelling law, modelled after one that had already been enacted in Chile, entered into effect in October 2020, requiring black stop signs on packages of foods high in added sugar, fats (saturated and trans fats), calories and added sodium. Nothing with black stop signs can be sold or promoted in schools, further protecting children.
Cambodia, Eswatini, Georgia, Jordan, Myanmar, Serbia andSri Lanka have made particular mention of the importance and relevance of tobacco control measures and/or implementation of the Framework Convention on Tobacco Control in their national COVID-19 response and recovery plans. Some international bodies are developing new One Health and Planetary Health approaches including policies for NCD prevention; for example, WHO’s Manifesto for a Healthy Recovery[36] and the European Union’s Beating Cancer Plan[37] which will address tobacco and alcohol as major risk factors.

© Framework Convention Alliance
RECOMMENDATION #7
Combat inequalities through better social protection
Leadership is needed to turn the tide on inequality. A widening health gap has been brought to the fore by the inequitable impacts of COVID-19 on different socio-economic groups and communities.[38] Disparities in healthy life expectancy for marginalised and deprived groups reveal disproportionate exposure to NCD risk factors and the structural barriers to health which have driven the syndemic of COVID-19 and NCDs.
COVID-19 continues to aggravate the inequalities that put some people at higher risk in every crisis, whether an epidemic, conflict or the impacts of climate change. Four decades of experience in combatting HIV/AIDS have shown the way: Policy action, community support and international cooperation to close health gaps and leave no one behind is the only way to end epidemics.
Governments and the global health and development community must identify the inequalities that largely determine who has access to healthy environments, and to health services and care which meet their needs, and who is denied and left behind. These barriers must be dismantled by laws, policies and social protection programmes designed to protect everyone, bringing everyone on board for the recovery. These include poverty, racism, discrimination, all forms of malnutrition (including overweight and obesity[39],[40]), insecure employment, poor education and housing, and unsafe or polluted environments, as well as barriers to access healthcare.
Inspiring example:
The Welsh government has made a focus on fairness central to their recovery plans, producing the Welsh Health Equity Status Report initiative (WHESRi) entitled: Placing health equity at the heart of the COVID-19 sustainable response and recovery: Building prosperous lives for all in Wales.[41]
We cannot waste a moment in shaping a society without the vulnerabilities that hindered our COVID response.”
Pillar 3
Health Systems: Fairer and fit for the future
Analyses of previous epidemics concluded that effective national health systems are the first line of defence. Health system resilience is defined as “the capacity of health actors, institutions, and populations to prepare for and effectively respond to crises; maintain core functions when a crisis hits; and, informed by lessons learned during the crisis, reorganise if conditions require it”.[42] This definition applies in the context of unforeseen disease outbreaks and disasters, but also the epidemiological transition to NCDs becoming the major causes of death and disease throughout all regions of the world. The major disruptions to essential NCD services caused by COVID-19 worldwide has highlighted that the lessons from previous epidemics had not been learned by the international community nor reflected in national governments’ investments in health systems.
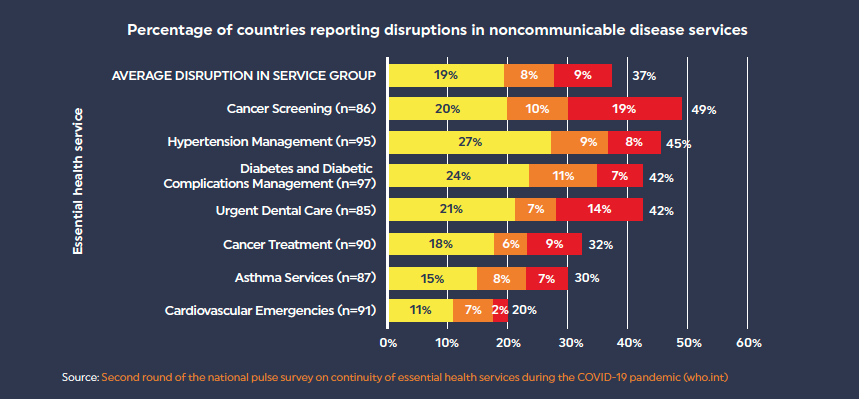
Nearly half of countries reported disruptions to one or more services for noncommunicable diseases
Preparedness for future health threats requires the ability of health systems to provide a swift surge response without putting the health of the wider population at risk. To enable this, health systems must be rebuilt stronger and fairer, on the foundation of comprehensive primary healthcare for all conditions, including NCDs which have historically been neglected.
COVID-19 has revealed the fragility of systems and capacities, and the longstanding under-resourcing of NCD essential services, public health, disease prevention and health promotion. Essential NCD services have been shown to lack resilience in almost all countries, indicated by severe disruptions to both routine and life-saving interventions, such as organ transplants or dialysis. Full services need to be urgently resumed. Governments must build back stronger and ensure that capacities are sustainably increased across the full continuum of care: health promotion, screening, diagnosis, treatment, rehabilitation and palliative care. In order to achieve this, governments will need to finally deliver on their previous commitments to health financing, health workforce and universal health coverage (UHC) and ensure social protection is in place to address the inequalities exacerbated by the pandemic. Health services often excluded from UHC must be integrated within the health system, including mental health, vision, hearing, and dental healthcare.
The global effort to respond to COVID-19 offers a valuable opportunity for synergies for better health and equity across all conditions and across the life course, so that people are included from early childhood through adulthood. As national health systems respond and the international community is mobilised to rapidly develop and deliver diagnostics, therapeutics, vaccines and essential supplies, new approaches can be anchored to provide lasting benefits to make health systems fit for purpose to respond to community health needs. Health systems cannot become resilient or responsive without the inclusion of NCD services and treatment in basic care packages (such as the WHO ‘PEN’ package of essential NCD interventions), and unless they become inclusive of everyone who needs care.
RECOMMENDATION #8
Integrate NCD services into the pandemic response and beyond
Health systems should adapt to support and manage the increased risks of infectious diseases and complications to people with known NCDs. Good practices developed during the pandemic can be maintained; for example, reducing health facility overcrowding and infection risk via patient triage, appointment scheduling, extended service hours and consultations across more locations, including community health centres.
Innovations should be made permanent to reduce the need to visit healthcare facilities, by encouraging telehealth consultations, home visits by community health workers (including mental health and oral health), multi-month prescriptions and easier prescription refills, home delivery of medicines, and support for self-care. In many countries, regulatory frameworks will need to be put in place to ensure these approaches are safe, effective and sustainably resourced over the longer term.
The pandemic response also offers an opportunity to reconfigure health systems for early detection, diagnosis and care for NCDs, alongside other chronic conditions. The roll-out of large-scale contact with communities can be used for opportunistic screening to close the diagnosis gap for common NCDs such as hypertension, diabetes, chronic respiratory disease, chronic kidney disease, oral diseases and mental health conditions, as well as communicable conditions such as tuberculosis or rheumatic fever. This can also be used to raise awareness among people at increased risk of NCDs during COVID-19 testing and/or immunisation programmes, particularly considering common risk factors including tobacco use and obesity. COVID-19 vaccination programmes could also be an opportunity to deliver vaccines for other viruses and infections, such as influenza and human papillomavirus immunisation for target populations. The latter would deliver on the targets of the Global Strategy to Eliminate Cervical Cancer.[43]
Inspiring examples:
In Bangladesh, district health information software used to monitor COVID-19 has also been customised to track the cervical cancer screening programme.[44]
In a number of countries, including Canada and Saudi Arabia, surveys and tools including applications have been deployed to monitor population wellbeing and mental health.[45] [46]
There has been particular outreach to population groups at higher risk of mental health conditions during the pandemic, including those shielding due to chronic health conditions in New York City[47] or frontline health professionals, in countries including China, Singapore, Japan, Italy, Saudi Arabia and Switzerland.[48]
In Australia, new guidelines have been developed for screening of gestational diabetes during COVID-19.[49]

© Md. Quamrul Ashan Shishir
RECOMMENDATION #9
Strengthen health services and primary care at the community level
Lessons learned during the pandemic are strengthening the call for integration of NCDs into communicable disease programmes and UHC, on the basis of the WHO PEN[50] package of essential NCD interventions in primary care and PEN-Plus[51] at first-level hospitals in low-resource settings.
The programmatic and funding silos in global health focusing on specific diseases or population groups must respond to the urgent need for broader strengthening of health systems on the basis of primary healthcare.[52] [53] The NCD Alliance has joined the Coalition of Partnerships for UHC and Global Health to work together across silos.[54] A new report from the World Bank outlines recommendations and offers support to governments in reforming the design and financing of primary care, integrated around patients’ needs, to “flatten the curve during health crises like COVID-19”.[55]
The pandemic has revealed fault lines between major urban centres and rural and Indigenous communities, including in gathering of mortality data in relation to the pandemic. This means that the true impact may still be far underestimated.[56] Decentralisation of care has considerably advanced during the pandemic in many countries and should be further supported. Offering care at home or at the local level so people can seek timely care is more cost-effective, for patients, families and governments. When healthcare is provided locally, travelling requirements are reduced, thus limiting the spread of infectious diseases, to which people living with NCDs are more vulnerable.
Inspiring examples:
Kenya aims to achieve UHC in 2022, including NCD prevention and care. The nation has already successfully piloted a UHC programme.
Investment in training of non-physician community health workers has proven effective for delivery of chronic care; for example in Rwanda, India, and Village Health Volunteers in Thailand.[57] Community health workers enjoy high levels of trust, so governments should invest to ensure they can support awareness-raising in self-management of chronic conditions, adherence to public health guidelines and uptake of vaccination campaigns, while providing essential primary care services and monitoring local population health.
I would request more funding for the primary healthcare areas so that NCDs are prevented or diagnosed timely to avoid the devastating complications. I would request that there is even distribution and decentralisation of NCD care across the country so that all people can receive treatment within their home areas, as travelling to major cities is an economic burden to most families.”
RECOMMENDATION #10
Anchor innovations in data and deployment of digital technologies
Without reliable data, public health interventions are unlikely to succeed and be sustainable. In many countries, people living with NCDs were required to present a medical record to demonstrate eligibility for COVID-19 vaccination, but often did not have paperwork.
In contrast, countries with national health insurance systems underpinned by health information infrastructure proved well-equipped for contract tracing, targeted risk communication and safety nets for vulnerable groups (including Vietnam, Costa Rica and the Indian state of Kerala[58]). The Africa Centres for Disease Control and Prevention (Africa CDC) launched a continent-wide COVID-19 surveillance system and daily dashboard, supported by US CDC, to inform national responses.[59]
Population-wide COVID-19 testing and vaccination offers a valuable opportunity to update health records and national data and significantly improve NCD-UHC indicators and monitoring. High quality, real-time data regarding NCD prevalence, co-morbidities and risk factor exposure is lacking in most countries, and often is only available with a considerable time lag. Results of opportunistic screening should be recorded at the same time as pandemic response data in digital platforms tracking vaccination rollout, to improve NCD data sets to inform future decision-making and ensure timely follow-up and continuity of care.
Significant leaps have been made during the pandemic towards the use of telehealth digital tools in healthcare, including those to support community health workers provide appropriate care and those to assist patients with self-management of chronic conditions.[60] Capabilities and applications designed to respond during the pandemic should be maintained and the regulatory frameworks updated to secure patient data and protect privacy, for example apps to facilitate telehealth consultation and to renew electronic prescriptions. Policy-makers, health systems and technology providers however need to be mindful of exacerbating the digital divide – and ensuring that measures are inclusive of those without devices, telephone or internet access.
Inspiring examples:
In Kenya and Nigeria, COVID-19 has catalysed rapid progress in telemedicine, including online video consultations with health professionals, home monitoring of blood glucose and blood pressure which can be relayed to health professionals, electronic prescriptions for local collection or delivery, and electronic scheduling of tests, for COVID-19 as well as NCDs and other conditions.
In Bangladesh and India, contextual digital platforms for managing hypertension have enabled actionable reporting and improved patient management. The Simple application, supported by Resolve to Save Lives, an initiative of Vital Strategies, aims to dramatically increase the number of people with hypertension who have their blood pressure measured and controlled. The app is now used by around 3,000 public health facilities, including district hospitals and community health services, and over 750,000 patients.[61]

© Resolve to Save Lives
RECOMMENDATION #11
Resolve bottlenecks in supply chains
The necessity of international coordination of worldwide distribution of diagnostics, therapeutics, vaccines and essential supplies to respond to COVID-19 was identified early in the pandemic. A call from G20 leaders mobilised global health institutions and donors to establish the Access to COVID-19 Tools Accelerator (ACT-A)ii, recognising that no one is safe until everyone is safe.
ACT-A is built on competencies developed over decades – particularly in HIV, TB and malaria responses – and new financing mechanisms and tools are being established to deliver necessary supplies, with a focus on equity. The innovations developed should be designed to contribute more broadly to longer term health systems strengthening, in order to provide lasting benefits for resilience and preparedness. In particular, the Health Systems Connector within ACT-A remains underresourced and its potential untapped. Coordination around health systems strengthening should become a higher priority as the response progresses.
Accessible, equitable supply chains reaching all countries and communities should be recognised as a global public good and accorded higher priority during and after the pandemic response. While COVID-19 vaccines have been developed, trialled, and produced at unprecedented speed and quantities, innovation in supply chains has not kept pace and they have proven a critical bottleneck hindering equitable access between countries and communities.
Prior to the pandemic, essential medicines and technologies (EMTs) for NCDs were already insufficiently available at health facilities in LMICs, where 85% of NCD deaths of people between 30-70 years old occur. This particularly affects the public sector, rural areas and lower levels of care, where NCD supplies are less available than those for acute illnesses. [62] Most LMICs are far off track for the WHO target to achieve 80 percent availability of essential NCD medicines and technologies in the public and private sectors by 2025. Ground-breaking progress in the distribution of diagnostics, therapeutics and vaccines for COVID-19 therefore also offers significant potential for NCDs. Synergies should be explored for diagnostics, testing programmes and data collection, to close the gap in NCD diagnosis and increase understanding of at-risk groups for COVID-19 and other infectious diseases.
Supply chain at the scale required for global population vaccination programmes appears to fall between the cracks between governments, programmes implemented by international institutions and civil society organisations, and logistics companies. International resources, capacitybuilding and technical assistance are urgently needed to tackle supply chain barriers and ensure COVID-19 vaccines reach every community. The No Empty Shelves initiative had already demonstrated that weak supply chains are a major barrier to access for NCD care in LMICs.[63] With EMTs for diabetes as an example, several critical barriers were identified in national public health supply chains: the need to improve quantitative forecasting and supply planning processes for EMTs, strengthen procurement capacity, support public authorities to more effectively negotiate purchase prices and limit mark-ups along the supply chain, and investigate feasibility of pooled procurement for NCD products.
In particular, challenges in the rollout of the ACT-A vaccine pillar, COVAX, have laid bare the absence of effective temperature-controlled supply chains, or cold chain, for most of the world. Cold chain improvements should be designed to deliver co-benefits for NCDs; for example, for a safe and quality-assured supply of insulin. However, to enable cold chain expansion, innovation will be needed to reduce and mitigate the significant climate impacts of refrigerants.
Huge gains could be made in LMICs for population health and health systems strengthening by realising synergies with the ACT-Accelerator to tackle longstanding supply chain barriers for NCD EMTs (including the essential medicines list for children), while engaging local communities to ensure adaptation to local needs.
Inspiring examples:
In Ghana and Rwanda, on-demand aerial delivery of urgent medical supplies to hospitals and health centres has been trialled in recent years with the aim of facilitating last mile delivery in areas where transport by road is slow.[64]
ii ACT-Accelerator partners: the Bill & Melinda Gates Foundation, CEPI, FIND, Gavi, The Global Fund, Unitaid, Wellcome, WHO, World Bank, plus UNICEF and PAHO as delivery partners for COVAX, the vaccines pillar.
RECOMMENDATION #12
Facilitate and support local production of essential NCD medicines
In addition to international supply chain innovations, COVID-19 has reinvigorated high-level discussion of local production of medicines and vaccines in LMICs. The World Health Assembly in May 2021 adopted a resolution on local production,[65] followed by political discussions on expanding manufacturing capacity. The WHOconvened World Local Production Forum aims to achieve alignment in the production of health products as safeguards to protect national, regional and global security.[66]
While vaccines are complex to produce, it has been proposed that relatively simpler essential medicines for NCDs could be produced in LMICs, as a gateway to develop permanent infrastructure, production facilities, workforce skills and necessary regulatory frameworks, which could be used to respond to future epidemics as needed. Feasibility and costeffectiveness should be examined regarding the development of production capacity in LMICs for essential NCD medicines based on community needs, such as insulin, blood glucose lowering medications, opioids for pain management, medication for hypertension, Benzathine penicillin G (BPG) to prevent rheumatic heart disease, etc. Safety, quality and efficacy would need to be assured. For this solution to deliver for smaller countries, including small island developing states, regional approaches should be explored. Capacity building would be needed for regional supply chains and last-mile distribution. The potential for LMIC production of NCD medicines as the starting point to install, develop and scale up necessary infrastructure and capacities, should be considered in negotiations for a pandemic treaty.
Inspiring example:
South Africa has become the first country to secure an agreement to host a technology transfer hub to produce mRNA vaccines, with guidance from Africa Centres for Disease Control and Prevention.
People-centred policy is the need of the hour. […] Together, we must reduce NCD risks and ensure all people have access to quality care and treatment that is equitable, comprehensive and affordable. Every opportunity must be grasped, and every innovation harnessed. No one can be left behind.[67]
References
01 Horton R. Offline: COVID-19 is not a pandemic. Lancet [Internet]. 2020 Sep 26;396(10255):874. Available from: https://doi.org/10.1016/S0140-6736(20)32000-6
02 NCD Countdown 2030. Available from: https://ncdcountdown.org
03 The Defeat-NCD Partnership. Implications of non-communicable diseases care policies on COVID-19 disease management. 2021. Available from: https://defeat-ncd.org/wp-content/uploads/2021/04/ Implications-of-non-communicable-diseases-care-policieson-COVID-19-disease-management_13-April-2021.pdf
04 Global SDG Integration, Impact of COVID-19 on the Sustainable Development Goals. Available from: https://sdgintegration.undp.org/accelerating-development-progressduring-covid-19
05 Horton R. Offline: COVID-19 is not a pandemic. Lancet [Internet]. 2020 Sep 26;396(10255):874. Available from: https://doi.org/10.1016/S0140-6736(20)32000-6
06 World Health Organization. WHO survey reveals NCD services are disrupted in Europe during pandemic. 2020 June. Available from: https://www.who.int/news-room/feature-stories/detail/who-surveyreveals-ncd-services-are-disrupted-in-europe-during-pandemic
07 Institute for Health Metrics and Evaluation. Estimation of excess mortality due to COVID-19. 2021 May. Available from: http://www.healthdata.org/special-analysis/estimation-excessmortality-due-covid-19-and-scalars-reported-covid-19-deaths
08 Shadmi E, Chen Y, Dourado I, Faran-Perach I, Furler J, Hangoma P, et al. Health equity and COVID-19: global perspectives. Int J Equity Health [Internet]. 2020;19(1):104. Available from: https://doi.org/10.1186/s12939-020-01218-z
09 Clark A, Jit M, Warren-Gash C, Guthrie B, Wang HHX, Mercer SW, et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Heal [Internet]. 2020 Aug 1;8(8):e1003–17. Available from: https://doi.org/10.1016/S2214-109X(20)30264-3
10 Haldane V, De Foo C, Abdalla SM, Jung A-S, Tan M, Wu S, et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med [Internet]. 2021;27(6):964–80. Available from: https://doi.org/10.1038/s41591-021-01381-y
11 UNGA Resolution A/RES/74/306. 2020;(September). Available from: https://documents-dds-ny.un.org/doc/UNDOC/GEN/N20/236/00/PDF/N2023600.pdf?OpenElement
12 Singh K, Kondal D, Mohan S, Jaganathan S, Deepa M, Venkateshmurthy NS, et al. Health, psychosocial, and economic impacts of the COVID-19 pandemic on people with chronic conditions in India: a mixed methods study. BMC Public Health. 2021 Apr;21(1):685.
13 NCD Child. Living with Type 1 Diabetes – Perspectives from Young People. 2021 May. Available from: https://www.ncdchild.org/2021/05/17/living-with-type-1-diabetes-perspectives-from-young-people/
14 The Independent Panel for Pandemic Preparedness and Response. No more pandemics! Bearing witness to COVID-19 and committing to a more secure future. 2021. Available from: https://live-the-independent-panel.pantheonsite.io/wpcontent/uploads/2021/06/NoMorePandemics_FINAL.pdf
15 World Health Organization. Voice, agency,empowerment – handbook on social participation for universal health care. 2021 May. Available from: https://www.who.int/publications/i/item/9789240027794
16 Financing for Global Commons for Pandemic Preparedness and Response. A Global Deal for Our Pandemic Age. 2021. Available from: https://pandemic-financing.org/report/foreword/
17 Allen LN. Financing national non-communicable disease responses. Glob Health Action. 2017;10(1):1326687. Available from: https://pubmed.ncbi.nlm.nih.gov/28604238/
18 ACTaccelerator. What is the Access to COVID-19 Tools (ACT) Accelerator, how is it structured and how does it work. 2021 April. Available from: https://www.who.int/publications/m/item/what-is-the-access-to-covid-19-tools-(act)-accelerator-how-is-it-structured-and-how-does-it-work
19 NCD Alliance, International Diabetes Federation and World Heart Federation. Pressure Points: Call for simultaneous action on diabetes and hypertension for more resilient health systems. 2021. Available from: https://ncdalliance.org/sites/default/files/resource_files/Pressure%20Points_Diabetes%20Brief_FINAL.pdf
20 Shroff ZC, Marten R, Vega J, Peters DH, Patcharanarumol W, Ghaffar A. Time to reconceptualise health systems. Lancet [Internet]. 2021 Jun 5;397(10290):2145. Available from: https://doi.org/10.1016/S0140-6736(21)01019-9
21 World Health Organization. COVID-19: Virtual Press conference. 2020 September. Available from: https://www.who.int/docs/default-source/coronaviruse/transcripts/covid-19-virtualpress-conference-4-september.pdf?sfvrsn=6504a1bd_2
22 Yang J, Hu J, Zhu C. Obesity aggravates COVID-19: A systematic review and meta-analysis. J Med Virol. 2021 Jan;93(1):257-261. Available from: https://pubmed.ncbi.nlm.nih.gov/32603481/
23 Marouf N, Cai W, Said KN, Daas H, Diab H, Chinta VR, et al. Association between periodontitis and severity of COVID-19 infection: A case-control study. J Clin Periodontol. 2021 Apr;48(4):483–91. Available from: https://pubmed.ncbi.nlm.nih.gov/33527378/
24 Lal A, Erondu NA, Heymann DL, Gitahi G, Yates R. Fragmented health systems in COVID-19: rectifying the misalignment between global health security and universal health coverage. Lancet [Internet]. 2021 Jan 2;397(10268):61–7. Available from: https://doi.org/10.1016/S0140-6736(20)32228-5
25 World Economic Forum. Action needed on causes of obesity to stop pandemic deaths. 2021 March. Available from: https://www.weforum.org/agenda/2021/03/actionneeded-causes-obesity-stop-future-pandemic-deaths/
26 SPECTRUM Consortium, NCD Alliance. Signalling Virtue, Promoting Harm - Unhealthy commodity industries and COVID-19. 2020 September. Available from: https://ncdalliance.org/resources/signalling-virtue-promoting-harm
27 European Commission. ‘Fit for 55’: delivering the EU’s 2030 Climate Target on the way to climate neutrality. 2021 July. Available from: https://ec.europa.eu/info/sites/default/files/chapeau_communication.pdf
28 European Commission. Transparency register. Available from:https://ec.europa.eu/info/about-european-commission/servicestandards-and-principles/transparency/transparency-register_en
29 Slum Dwellers International. Enhancing the Resilience of Slum Communities to Overcome the Covid-19 Crisis. 2021 February. Available from: https://sdinet.org/2021/02/enhancing-the-resilienceof-slum-communities-to-overcome-the-covid-19-crisis/
30 NCD Alliance, International Diabetes Federation and World Heart Federation. Pressure Points: Call for simultaneous action on diabetes and hypertension for more resilient health systems. 2021. Available from: https://ncdalliance.org/sites/default/files/resource_files/Pressure%20Points_Diabetes%20Brief_FINAL.pdf
31 Singh K, Kondal D, Mohan S, Jaganathan S, Deepa M, Venkateshmurthy NS, et al. Health, psychosocial, and economic impacts of the COVID-19 pandemic on people with chronic conditions in India: a mixed methods study. BMC Public Health. 2021 Apr;21(1):685.
32 Francis A, Baigent C, Ikizler TA, Cockwell P, Jha V. The urgent need to vaccinate dialysis patients against severe acute respiratory syndrome coronavirus 2: a call to action. Kidney Int [Internet]. 2021 Apr 1;99(4):791–3. Available from: https://doi.org/10.1016/j.kint.2021.02.003
33 World Health Organization, Regional Office for Europe. Nutrition - Prevention and control of NCDs at core of COVID-19 response. 2020 June. Available from: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/news/news/2020/6/prevention-and-control-of-ncds-at-core-of-covid-19-response
34 World Health Organization. ‘Best Buys’ and Other Recommended Interventions for the Prevention and Control of Noncommunicable Diseases. Updated (2017) Appendix 3 of the Global Action Plan for the Prevention and Control of Nonocommunicable Diseases 2013-2020. Available from: https://www.who.int/ncds/management/WHO_Appendix_BestBuys_LS.pdf
35 Resolve to Save Lives, Vital Strategies. Building resilient populations in the face of COVID-19. Available from: https://preventepidemics.org/wp-content/uploads/2020/12/013_RTSL_COVID_Covid-and-NCDS-Building-Relilient-Populations_Fact-Sheet_1120_Rev-A_v3-3.pdf
36 World Health Organization. WHO Manifesto for a Healthy Recovery from COVID-19: Prescriptions and Actionables for a Healthy and Green Recovery. 2020. Available from: https://www.who.int/docs/default-source/climate-change/whomanifesto-for-a-healthy-and-green-post-covid-recovery.pdf
37 European Commission. Non-communicable diseases: Cancer. Available from : https://ec.europa.eu/health/non_communicable_diseases/cancer_en
38 The Health Foundation. Health Equity in England: The Marmot Review 10 Years On. 2020 February. Available from: https://www.health.org.uk/publications/reports/the-marmot-review-10-years-on
39 The International Policy Centre for Inclusive Growth. Policy in Focus. Volume 18, Issue 1. 2020 December. Available from http://www.fao.org/3/cb2498en/CB2498EN.pdf
40 Alderman H. Leveraging Social Protection Programs for Improved Nutrition: Summary of Evidence Prepared for the Global Forum on Nutrition-Sensitive Social Protection Programs. 2015. Available from: https://openknowledge.worldbank.org/ bitstream/handle/10986/24450/K8701.pdf?sequence=4
41 World Health Organization Collaborating Centre on Investment for Health and Well-being, Public Health Wales, Welsh Government. Placing health equity at the heart of the COVID-19 sustainable response and recovery: Building prosperous lives for all in Wales. 2021. Available from: https://phwwhocc.co.uk/wp-content/uploads/2021/07/WHESRi-Covid-Report-Eng.pdf
42 Kruk ME, Myers M, Varpilah ST, Dahn BT. What is a resilient health system? Lessons from Ebola. Lancet 2015; 385: 1910–12. Available from: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)60755-3/fulltext
43 World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem. 2020 November. Available from: https://www.who.int/publications/i/item/9789240014107
44 Basu P, Lucas E, Zhang L, Muwonge R, Murillo R, Nessa A. Leveraging vertical COVID-19 investments to improve monitoring of cancer screening programme – A case study from Bangladesh.Prev Med (Baltim) [Internet]. 2021;151:106624. Available from: https://www.sciencedirect.com/science/article/pii/S0091743521002085
45 Strudwick G, Sockalingam S, Kassam I, Sequeira L, Bonato S, Youssef A, et al. Digital Interventions to Support Population Mental Health in Canada During the COVID-19 Pandemic: Rapid Review. JMIR Ment Heal. 2021 Mar;8(3):e26550. Available from: https://pubmed.ncbi.nlm.nih.gov/33650985/
46 BinDhim NF, Althumiri NA, Basyouni MH, Alageel AA, Alghnam S, Al-Qunaibet AM, et al. Saudi Arabia Mental Health Surveillance System (MHSS): mental health trends amid COVID-19 and comparison with pre-COVID-19 trends. Eur J Psychotraumatol. 2021 Feb;12(1):1875642. Available from: https://pubmed.ncbi.nlm.nih.gov/34025918/\
47 Pizzirusso M, Carrion-Park C, Clark US, Gonzalez J, Byrd D, Morgello S. Physical and Mental Health Screening in a New York City HIV Cohort During the COVID-19 Pandemic: A Preliminary Report. J Acquir Immune Defic Syndr. 2021 Mar;86(3):e54–60. Available from: https://pubmed.ncbi.nlm.nih.gov/33148994/
48 Weibelzahl S, Reiter J, Duden G. Depression and anxiety in healthcare professionals during the COVID-19 pandemic. Epidemiology and Infection. Cambridge University Press; 2021;149:e46. Available from: https://www.cambridge.org/core/journals/epidemiology-and-infection/article/depressionand-anxiety-in-healthcare-professionals-during-the-covid19-pandemic/FBAD40732F4A587B814DA418DF9A5593
49 Australasian Diabetes in Pregnancy Society, Australian Diabetes Society, Australian Diabetes Educators Asswocation, Diabetes Australia. Diagnostic testing for gestational diabetes mellitus during the COVID-19 pandemic: Antenatal and postnatal testing advice. 2020 May. Available from: https://www.diabetesaustralia.com.au/wp-content/uploads/Diagnostic-Testing-for-Gestational-Diabetes-during-COVID-19-advice.pdf
50 World Health Organization. Integrated management of NCDs. Available from: https://www.who.int/activities/integrated-management-of-ncds#:~:text=The%20WHO%20Package%20of%20essential%20noncommunicable%20%28PEN%29%20disease,low-resource%20settings%20for%-20the%20integrated%20management%20of%20NCDs.
51 Partners in Health, NCD Synergies. PEN-Plus Toolkit. Available from: http://ncdsynergies.org/chronic-care-toolkit/
52 De Maeseneer J, Li D, Palsdottir B et al. Universal health coverage and primary health care: the 30 by 2030 campaign; Bull World Health Organ 2020;98:812–814. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7607468/
53 Lal A, Erondu NA, Heymann DL, Gitahi G, Yates R. Fragmented health systems in COVID-19: rectifying the misalignment between global health security and universal health coverage. Lancet [Internet]. 2021 Jan 2;397(10268):61–7. Available from: https://doi.org/10.1016/S0140-6736(20)32228-5
54 UHC2030. The Coalition of Partnerships for UHC and Global Health. Available from: https://www.uhc2030.org/what-we-do/voices/advocacy/the-coalition-of-partnerships-for-uhc-and-global-health/
55 The World Bank. Well-designed Primary Health Care Can Help Flatten the Curve during Health Crises like COVID-19. 2021 June. Available from: https://www.worldbank.org/en/news/press-release/2021/06/28/well-designed-primary-health-carecan-help-flatten-the-curve-during-health-crises-like-covid-19
56 International Society of Nephrology. The Global Kidney Policy Forum 2021: Focus on North America and the Caribbean. Available from: https://www.theisn.org/wp-content/uploads/media/GKPF%202021%20Summary%20Pamphlet.pdf?p=adv
57 World Health Organization. Thailand's 1 million village health volunteers - “unsung heroes” - are helping guard communitiesnationwide from COVID-19. 2020 August. Available from: https://www.who.int/thailand/news/feature-stories/detail/thailands-1-million-village-health-volunteers-unsung-heroesare-helping-guard-communities-nationwide-from-covid-19
58 Lal A, Erondu NA, Heymann DL, Gitahi G, Yates R. Fragmented health systems in COVID-19: rectifying the misalignment between global health security and universal health coverage. Lancet [Internet]. 2021 Jan 2;397(10268):61–7. Available from: https://doi.org/10.1016/S0140-6736(20)32228-5
59 Centers for Disease Control and Prevention. Africa CDC Launches Continent-wide Response. 2020 December. Available from: https://www.cdc.gov/globalhealth/healthprotection/fieldupdates/fall-2020/africa-cdc-covid.html
60 World Health Organization. Second round of the national pulse survey on continuity of essential health services during the COVID-19 pandemic. 2021 April. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS-continuity-survey-2021.1
61 Resolve to Save Lives. Simple. Available from: https://www.simple.org/about/
62 PATH. No Empty Shelves: Diabetes Supplies: Are they there when needed? 2015. Available from: https://path.azureedge.net/media/documents/NCD_nes_long_rpt.pdf
63 PATH. No Empty Shelves: Diabetes Supplies: Are they there when needed? 2015. Available from: https://path.azureedge.net/media/documents/NCD_nes_long_rpt.pdf
64 e.g. Zipline. Available from: https://flyzipline.com/how-it-works/
65 Seventy-Fourth World Health Assembly. Resolution WHA74.6: Strengthening local production of medicines and other health technologies to improve access. 2021 May. Available from: https://apps.who.int/gb/ebwha/pdf_files/WHA74/A74_R6-en.pdf
66 World Health Organization. World Local Production Forum. Available from: https://www.who.int/initiatives/world-local-production-forum
67 Bangkok Post. Ramp up action against NCDs. 2021 June. Available from: https://www.bangkokpost.com/opinion/opinion/2137491/ramp-up-action-against-ncds



