20 things you should know about mental health today

The World Health Organization has just released the World Mental Health Report, a follow-up to a 2001 study. Here are 20 things you should know about the state of mental health globally.
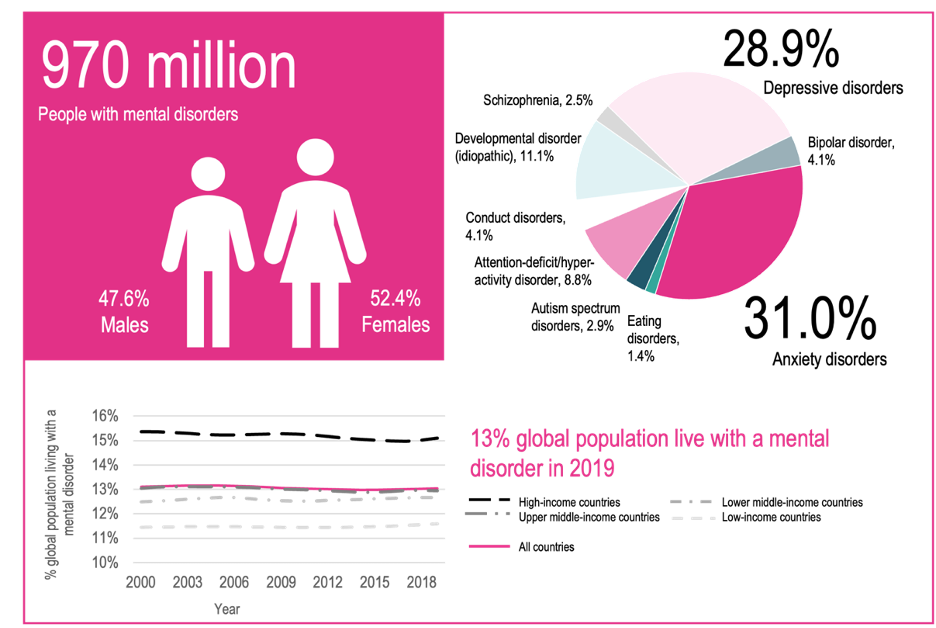
1. Mental disorders are common
Nearly a billion people around the world (1/8) live with a diagnosable mental disorder. In all countries, mental health conditions are highly prevalent. The prevalence of different mental disorders varies with gender and age. In both males and females, anxiety disorders and depressive disorders are the most common.
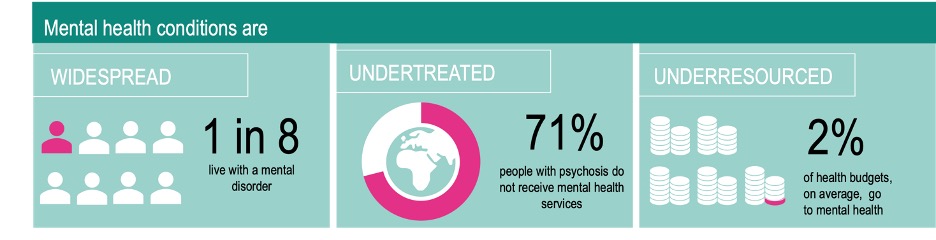
2. Neither mentally healthy nor mentally ill
We are not either mentally healthy or mentally ill. Mental health exists on a complex continuum, with experiences ranging from an optimal state of well-being to states of great suffering and emotional pain. So mental health is not defined by the presence or absence of mental disorder.
Although people with mental health conditions are more likely to experience lower levels of mental well-being, this is not always the case. Just as someone can have a physical health condition and still be physically fit, so people can live with a mental health condition and still have high levels of mental well-being.
3. Females and males
Depressive and anxiety disorders are about 50% more common among women than men, while men are more likely to have a substance use disorder. As depressive and anxiety disorders account for most cases of mental disorder, overall, more women (13.5% or 508 million) than men (12.5% or 462 million) live with a mental disorder.
Women who have experienced intimate partner violence or sexual violence are particularly vulnerable to developing a mental health condition, with significant associations found
between victimization and depression, anxiety, stress conditions, and suicidal thoughts.
4. Life expectancy
People with severe mental health conditions – including schizophrenia and bipolar disorder – die on average 10 to 20 years earlier than average. Most of these deaths are due to preventable diseases, especially cardiovascular disease, respiratory disease and infection, which are more common in people with mental health conditions. In these cases, having a mental health condition may not be the cause of death, but it is likely to be a major contributing factor.
5. Rich or poor country?
More than 80% of all people with mental disorders live in low- and middle-income countries. There, the vicious cycle between mental health and poverty is particularly prevalent because of a lack of welfare safety nets and poor access to effective treatment.
Two-thirds of low-income countries reporting to WHO in 2020 did not include mental health care in national health insurance schemes. This means that people in need have to fund
their care themselves, often spending large and potentially impoverishing sums out of pocket.
6. Too little is being done
“The truth is that two decades after the landmark 2001 report, and nearly a decade after the world committed to the action plan, the countries and communities that have seen real innovation and advances remain islands of good practice in a sea of need and neglect,” says the report.
On average, countries dedicate less than 2% of their health care budgets to mental health. More than 70% of mental health spending in middle-income countries goes towards running stand-alone inpatient psychiatric hospitals. Around half the world's population lives in countries where there is just one psychiatrist to serve 200,000 or more people.
Close to 15% of the world’s working population is estimated to have a mental disorder at any given time. Researchers estimate that 12 billion workdays are lost every year to depression and anxiety alone, at a cost of nearly US$ 1 trillion. This includes days lost to absenteeism, presenteeism (when people go to work but underperform) and staff turnover.
7. Many people are untreated
A large proportion of people with diagnosed mental health conditions go completely untreated. WHO estimates that only 29% of people with psychosis — a condition where a person loses some contact with reality — receive mental health services.
8. Links to noncommunicable diseases
The four greatest risk factors for NCDs – tobacco use, unhealthy diets, physical inactivity and harmful use of alcohol – are all linked with various mental health conditions. Childhood adversity, which is a major risk factor for later-life mental health conditions, is similarly related to a range of adult-onset NCDs, including heart disease, diabetes and asthma.
9. Leading cause of disability
Mental disorders are the leading cause of years lived with disability — accounting for one in every six YLDs globally. Schizophrenia is a primary concern: in its acute states it is the most impairing of all health conditions. People with schizophrenia or other severe mental health conditions die on average 10 to 20 years earlier than the general population, often of preventable physical diseases.
10. Children & adolescents
Around 8% of the world’s young children (aged 5-9 years) and 14% of adolescents (aged 10-19 years) live with a mental disorder. A seminal nationwide study in the United States found that half of the mental disorders present in adulthood had developed by the age of 14 years; three-quarters appeared by the age of 24 years.
Globally, more than half of all children aged 2-17 (around 1 billion individuals) experienced emotional, physical or sexual violence in the previous year. Adverse childhood experiences, including exposure to violence, increase the risk of developing a wide range of behavioural problems and mental health conditions. These include substance use, aggression, depression, anxiety and post-traumatic stress disorder.
11. Suicide
Suicide affects people and their families from all countries and contexts, and at all ages. Globally, there may be 20 suicide attempts to every one death, and yet suicide still accounts for more than one in every 100 deaths. It is a major cause of death among young people.
Suicide prevention is an international priority, with a Sustainable Development Goal (SDG) target to reduce the suicide mortality rate by one-third by 2030.
12. Schizophrenia & bipolar disorder
Schizophrenia, which occurs in 24 million people and in approximately 1 in 200 adults (aged 20 years and over), is a primary concern of mental health services in all countries. In its acute states, it is the most impairing of all health conditions. Bipolar disorder, another key concern of mental health services around the world, occurs in 40 million people and approximately 1 in 150 adults globally in 2019. Both disorders primarily affect working-age populations.
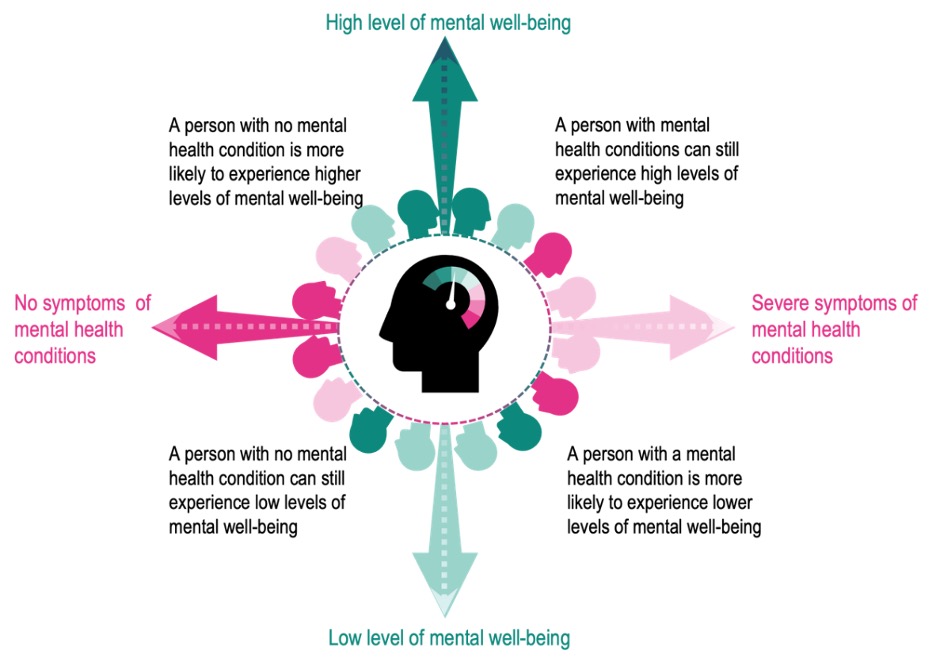
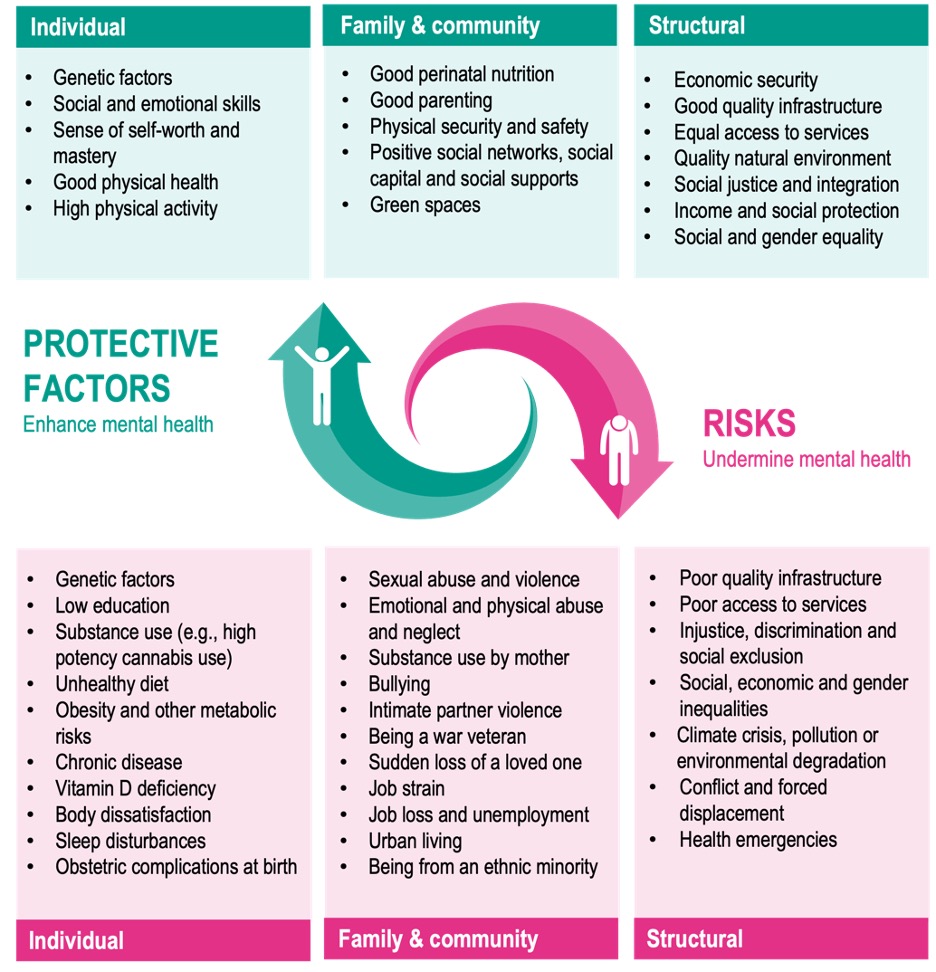
13. Poverty, violence, inequality — all risk factors
Indeed, at all ages and stages of life, adversity – including poverty, violence, inequality and environmental deprivation – is a risk to mental health. People who live in adverse conditions, such as war zones, experience more mental health conditions than people who do not.
Mental ill health is closely linked to poverty in a vicious cycle of disadvantage. This disadvantage starts before birth and accumulates throughout life. People living in poverty can lack the financial resources to maintain basic living standards; they have fewer educational and employment opportunities; they are more exposed to adverse living environments; and they are less able to access quality health care. These daily stresses put people living in poverty at greater risk of experiencing mental health conditions.
14. Impacts of environmental harm
Living in areas where the natural environment has been compromised – for example, throughclimate change, biodiversity and habitat loss, exploitation or pollution – can also undermine mental health. For example, growing evidence suggests that exposure to air pollution is likely to adversely affect the brain and increase the risk, severity and duration of mental health conditions at all stages of life.
Various terms hav e emerged to describe the psychological reactions people experience, including “climate change anxiety”, “solastalgia”, “eco-anxiety”, “environmental distress”, and many others. Whatever the label, the anxiety and despair felt, increasingly reported by young people, can be considerable and may put people at risk of developing mental health conditions.
15. Marginalised groups at risk
Socially marginalised groups – including the long-term unemployed, sex workers, homeless people and refugees – tend to have higher rates of mental disorder than the general population but can have difficulties in accessing health care.
16. Conflict
One in five people living in settings affected by conflict in the preceding 10 years is estimated to have depression, anxiety, PTSD, bipolar disorder or schizophrenia. Mental health conditions are also estimated to be very common among survivors of natural disasters. Experiencing a disaster increases the risk of problematic substance use, especially among people with pre-existing problems. Frontline responders, such as emergency care providers and relief workers, are at particular risk of mental health problems, both in the short and long term.
17. COVID-19
The COVID-19 pandemic has created a global crisis for mental health, fuelling short- and long-term stresses and undermining the mental health of millions. As part of the Global Burden of Diseases, Injuries and Risk Factors Study 2020, researchers estimated a 25-27% rise in the prevalence of depression and anxiety in the first year of the pandemic. A recent WHO umbrella review confirmed a significant rise, especially during the initial months of the pandemic. At the same time, mental health services have been severely disrupted and the treatment gap for mental health conditions has widened.
18. Global action plan
In 2013, WHO Member States adopted the Comprehensive mental health action plan 2013-2030. They committed to meet global targets for improved mental health. These were focused on strengthening leadership and governance, community-based care, promotion and prevention, and information systems and research.
19. From tragedy to support
Many countries have capitalized on emergency situations to build better mental health systems. In Sri Lanka, the impacts of the Asian tsunami in 2004 dramatically increased the political interest in mental health. This led to the mobilization of immediate resources for emergency mental health care, which then provided a platform for broader national mental health reform.
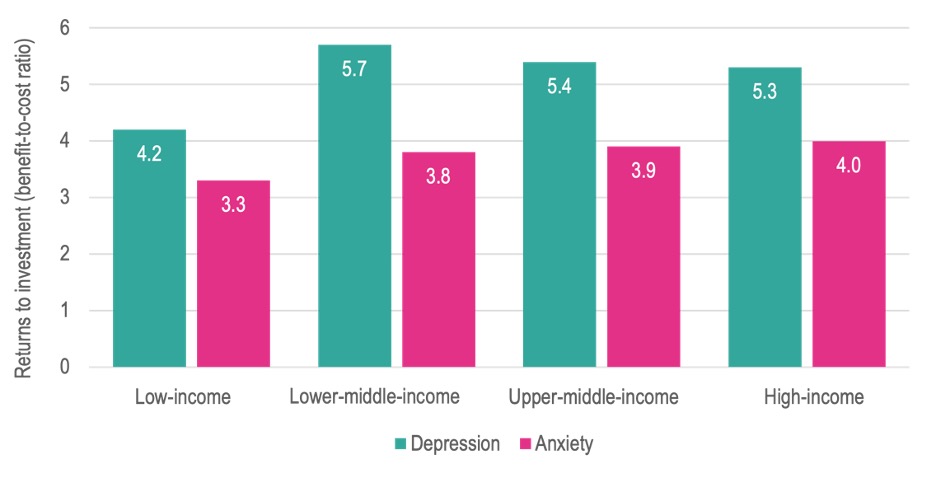
20. Investment pays off
One study of 36 countries found that every dollar invested in treating depression and anxiety generated five times the benefits in extra years of healthy life and in productivity.